Heart Failure Program
Transforming the Cardiac-Care Landscape
The new, cutting-edge Heart Failure Program at Good Samaritan Hospital, part of the Westchester Medical Center Health Network (WMCHealth), is the only one of its kind in Rockland and Orange counties. It brings unmatched, timely cardiac expertise right to communities where patients live.
The program offers the most contemporary therapies and unparalleled access to specialized physicians and life-saving care.
Services are provided by the nationally renowned WMCHealth Heart and Vascular Institute, also a member of WMCHealth. Its multidisciplinary heart failure team is comprised of heart failure physicians, cardiothoracic surgeons, advanced practitioners, psychiatrists, social workers and nutritionists who collaborate to optimize patient care.
Early identification and intervention are critical. Physicians optimize care of all aspects of heart failure from diagnosis to treatment and aftercare. This includes rapid evaluation for life-saving therapies such as mechanical circulatory support and transplant. Interventional cardiologists perform a full spectrum of diagnostic testing and catheterizations. They include rotoblade atherectomies, balloon angioplasties, radial catheterizations, extracorporeal membrane oxygenation and ventricular assist device implantation.
Advice From Medical Director, Alan L. Gass, MD, FACC
A New Heart Failure Treatment Device
An implantable therapeutic device is now available to treat individuals living with heart failure at Good Samaritan Hospital, a member of the Westchester Medical Center Health Network. This pacemaker-like device transmits electrical impulses to the brain and regulates cardiovascular function, which can lessen heart failure symptoms and can improve quality of life.
It is not a pacemaker or defibrillator; it is a therapy that “outsmarts” the heart by actively stimulating natural sensors in the body that tells the brain how to regulate the heart — which can relieve the symptoms of heart failure. Barostim™ (Baroreflex Activation Therapy) is the first FDA-approved implantable device that uses the power of the autonomic nervous system to help improve symptoms of heart failure. It works by stimulating baroreceptors – natural sensors in the body that tell the nervous system how to regulate heart, kidney and vascular function. These effects can reduce the heart’s workload and help it pump more efficiently, helping to relieve the symptoms of heart failure.
This procedure typically takes less than an hour and patients usually go home the same day. It’s the only heart failure device therapy that does not require any hardware in the heart or blood vessels. Once implanted, our physicians schedule routine follow-ups to ensure that device settings are optimized to best improve heart failure symptoms.
Who Qualifies for this Procedure?
Diagnosed with heart failure? – Patients who have been diagnosed with heart failure and whose heart has an “ejection fraction” of 35 percent or less.
Prescribed heart medicine? – Patients who are taking heart failure medications prescribed by their cardiologist.
Symptoms impact your daily life? - Despite the medication, the heart failure symptoms significantly impact a patient’s daily life and reduces his or her activities.

Gunjan Shukla, MD, Clinical Director of Cardiac Electrophysiology, and Cardiothoracic Surgeon Chirag Badami, MD demonstrate how the device works with Joseph Carozza, 76, of Hopewell Junction, NY, the first patient to undergo this minimally-invasive procedure at Good Samaritan Hospital.
Hear from Our Patients

An Air Force Vet Survives a Double-Organ Transplant Thanks to This Strong Collaboration
The combined effort between Good Samaritan Hospital and Westchester Medical Center helps facilitate a double-organ transplant.
By David Levine
For more than two decades, Cary Hirsch, MD, helped keep Nelson Cintron alive. Dr. Hirsch, an interventional cardiologist and Director of the Cardiovascular Institute at Good Samaritan Hospital, a member of the Westchester Medical Center Health Network (WMCHealth), in Suffern, had been treating Nelson “since before the computer,” he says, for a variety of heart problems.
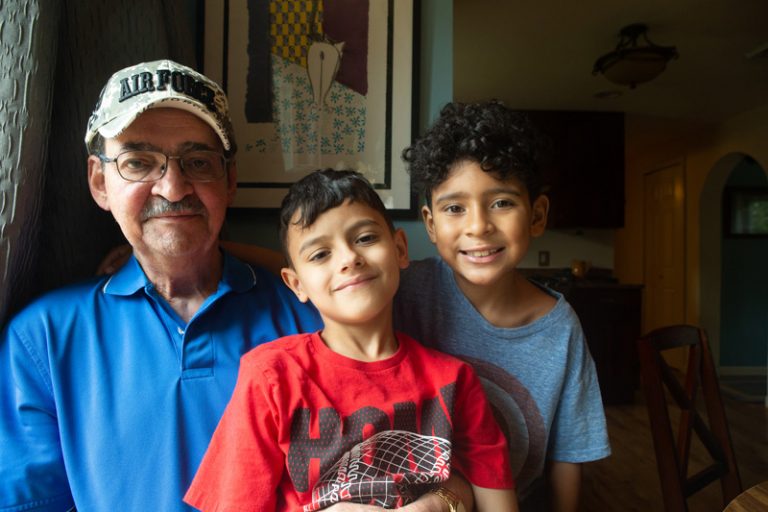
Nelson, 67, lives in New Hampton with his wife, Edna; they have one son and three grandchildren. He was diagnosed with cardiomyopathy — an enlarged heart — in 1995. Then, in 1999, his aortic valve failed, disrupting the function of his left ventricle, the main pumping chamber of the heart. He underwent valve replacement, which usually improves heart-muscle function dramatically. “In Nelson’s case, it improved only a bit and over time deteriorated,” Dr. Hirsch says.
To make matters worse, Nelson also developed an irregular heartbeat, or arrhythmia, and required the implantation of a pacemaker and defibrillator in 2005. Despite multiple procedures and interventions, Nelson’s heart continued to worsen. And then another problem arose: Nelson’s many heart medications over the years had taken a toll on his kidneys, which began to fail. “His medication dosages had to be lowered or not used at all, because they can cause the kidneys to worsen,” Dr. Hirsch says. “As doctors, we are caught between a rock and a hard place.”
Nelson’s health declined. “About a year ago, things got really bad,” he says. “I couldn’t breathe or get around. I got the flu and ended up at the hospital, in complete heart failure. When my kidneys started to go, Dr. Hirsch told me the only answer was a heart-and-kidney transplant.”
This is where Nelson’s fortunes turned. Dr. Hirsch took advantage of the newly formed Heart Failure collaboration between Good Samaritan Hospital and Westchester Medical Center, the flagship of WMCHealth. This program facilitates patients at Good Samaritan Hospital to be seen in Suffern by Westchester Medical Center specialists. Nelson was one of the first patients to be cared for through this program. Avi Levine, MD, who specializes in advanced heart failure and cardiac transplantation, took charge of his case, and Dr. Hirsch, who had developed a close relationship with Nelson over the years, continued to be involved, making the transition much more comfortable for Nelson.
“The advantage of having this program at a place like Good Samaritan Hospital is that it extends our reach,” Dr. Levine says. “For him to come to Westchester would have been challenging.” Each of the four specialists on the team spend a week at a time at Good Samaritan Hospital, to provide patients access to the advanced treatments offered through the WMCHealth Heart and Vascular Institute, which gives the patients access to the best physicians and researchers in cardiology, cardiovascular surgery, cardiothoracic surgery and pediatric cardiovascular services. “There is no advanced-heart-failure team in that area, except for Westchester Medical Center, so having our team there provides a level of care that these patients would not otherwise be able to conveniently access,” Dr. Levine says.
Nelson was later transferred to Westchester Medical Center for advanced evaluations of his heart and kidneys and put on more powerful medications to help his heart pump stronger. Nelson needed both a heart and a kidney, and both organs had to come from the same donor, to reduce the risk of rejection.
Nelson was ultimately accepted and listed as a transplant candidate, and after another hospital admission for worsening symptoms, he was kept in the hospital on high-dose intravenous medications to help his heart pump while awaiting a donor match. About 40 days later, those organs became available, and in March, he underwent surgery to save his life. The heart was transplanted first, and 24 hours later, he received a new kidney.

Dr. Levine and his team managed Nelson’s care after surgery. “The first six weeks were pretty tough,” Nelson admits. The pain wasn’t only physical. “A lot of things go through your mind when you’re lying in a room by yourself. You feel like you cheated death. A lot of emotions go through your head.”
Eventually he was sent to the cardiac rehabilitation unit at Westchester Medical Center, where he spent about a week regaining his strength — and some of the 40 pounds he’d lost. “I wanted to go home,” he says. “I missed my grandkids. Four months in the hospital is long enough.”
Once home, visiting nurses came to supervise his recovery, and he continued physical therapy for about two months. “Every day I felt a little better,” he says. “Now I feel pretty good.”
He visits Westchester Medical Center regularly for follow-up biopsy procedures. in addition to regular visits to Good Samaritan Hospital for routine follow-up care. His results have been excellent.
The best days, he says, are when the grandchildren visit. “Keeping up with a 3-year-old and two 7-year-olds is a job,” he says, but thanks to his new lease on life, he’s up to the task. “Before, by the time I got to the top of eight steps, I had to hold on to something, and I couldn’t breathe,” he says. “Now, no problem.”
While Nelson’s health has improved dramatically, he is still grappling with powerful emotions. “You realize you are walking around with two organs you weren’t born with. It gets complicated. You think about your responsibility to the donor family. They are like a second mother. They gave me life.”
Meet Our Team:
Heart Failure Program Specialists
Alan L. Gass, MD, FACC, is Medical Director of Cardiac Transplantation and Mechanical Circulatory Support at Westchester Medical Center, as well as Professor of Medicine at New York Medical College. He graduated from The University of Medicine and Surgery in Sassari, Italy. He completed his residency at Long Island Jewish Medical Center and fellowships at Newark Beth Israel Medical Center in Newark, NJ, and Stanford University Hospital in Palo Alto, CA.
Gregg Lanier, MD, FACC, is the Director of Pulmonary Hypertension, Associate Director of Heart Failure, and Director of the Advanced Heart Failure and Transplant Cardiology Fellowship at Westchester Medical Center. He also is Assistant Professor of Medicine at New York Medical College. His medical degree is from Northwestern University; his residency was at Mount Sinai Hospital; and his fellowships were at Mount Sinai Hospital and Columbia-New York Presbyterian Hospital.
Chhaya Aggarwal Gupta, MD, FACC, graduated from Maulana Azad Medical College in New Delhi, India. Her residency was at Georgetown University Hospital, and her cardiovascular medicine fellowship was at the University of Arkansas for Medical Sciences. She completed her fellowship in Advanced Heart Failure and Transplantation at Cedars Sinai Medical Center in Los Angeles.
Elliot (Avi) Levine, MD, FACC graduated from Harvard Medical School in Boston. He completed his residency, cardiac fellowship and advanced heart failure and transplantation fellowship at Mount Sinai Hospital in New York City. He has co-authored numerous scholarly publications for The Journal of Nuclear Medicine, The Journal of Nuclear Cardiology and Pacing and Clinical Electrophysiology.
- Internal Medicine, Advanced Heart Failure and Transplant Cardiology
- Internal Medicine, Advanced Heart Failure and Transplant Cardiology
- Internal Medicine, Advanced Heart Failure and Transplant Cardiology
- Internal Medicine, Cardiovascular Disease
- Internal Medicine, Advanced Heart Failure and Transplant Cardiology
- Tele-ICU
,